Uveal tract is the vascular middle coat of the eye ball. Inflammation of the uveal tract is called uveitis. Uveitis, usually occurs if there is associated systemic disease in the patient either an autoimmune disease or an infectious disease.
What is Uveitis?
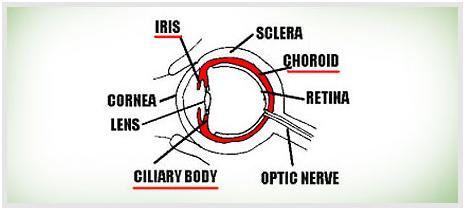 If we think of the eye as a hollow, fluid-filled, 3-layered ball then the outer layer is the sclera a tough coat, the innermost is the retina the thin light-gathering layer and the middle layer is the Uvea. The Uvea is made up of the iris, the ciliary body and the choroid (see diagram). When any part of the uvea becomes inflamed then it is called Uveitis. A big dilemma, when trying to understand Uveitis for patients and doctors alike is that there are many different types of Uveitis. This is because the Uvea is made up of different parts. So if the iris is affected the condition and its treatment could be totally different to when the choroid is affected. The inflammation in the Uvea very often affects other parts of the eye such as the retina so a variety of other problems can occur and complicate the picture. . Also there are a large number of medical conditions where Uveitis features amongst the symptoms of other diseases, for instance; Behcet's Disease, Sarcoidosis and Toxoplasmosis to name just three. So as can be seen there are many different types of causes of Uveitis. The term intraocular inflammation is often used to cover the spectrum of uveitis conditions. As there is a wide variety of different conditions and complications, it follows that there are numerous ways that it presents itself. The degree and type of sight loss and the type of treatment may vary considerably from patient to patient. Although the potential for confusion sounds high, as long as it is remembered that Uveitis is actually a number of different conditions then it is possible to find out about each individual case. It is of course very important for both patients and doctors to establish the exact type of Uveitis as far as possible and as early as possible
If we think of the eye as a hollow, fluid-filled, 3-layered ball then the outer layer is the sclera a tough coat, the innermost is the retina the thin light-gathering layer and the middle layer is the Uvea. The Uvea is made up of the iris, the ciliary body and the choroid (see diagram). When any part of the uvea becomes inflamed then it is called Uveitis. A big dilemma, when trying to understand Uveitis for patients and doctors alike is that there are many different types of Uveitis. This is because the Uvea is made up of different parts. So if the iris is affected the condition and its treatment could be totally different to when the choroid is affected. The inflammation in the Uvea very often affects other parts of the eye such as the retina so a variety of other problems can occur and complicate the picture. . Also there are a large number of medical conditions where Uveitis features amongst the symptoms of other diseases, for instance; Behcet's Disease, Sarcoidosis and Toxoplasmosis to name just three. So as can be seen there are many different types of causes of Uveitis. The term intraocular inflammation is often used to cover the spectrum of uveitis conditions. As there is a wide variety of different conditions and complications, it follows that there are numerous ways that it presents itself. The degree and type of sight loss and the type of treatment may vary considerably from patient to patient. Although the potential for confusion sounds high, as long as it is remembered that Uveitis is actually a number of different conditions then it is possible to find out about each individual case. It is of course very important for both patients and doctors to establish the exact type of Uveitis as far as possible and as early as possible

