A clinical condition characterised by thinning and forward protrusion of the cornea resulting in conical shape. This disorder is usually bilateral, with onset at the age of 10 -14 years. Affects both sexes, with a slight female preponderance. Although it has been reported in families, the risk of inheritance is reasonably low.
Why does it occur ?
Etiology of this condition is still not clear. . Eye rubbing, hormonal variations , genetic predisposition have been proposed to be causative factors in the disease. It is possible that this condition could be secondary to increased breakdown of the stromal collagen lamellae by the lysosomal enzymes released by the basal epithelium in these eyes.
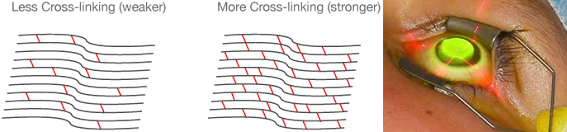
The substance of the cornea consists of hundreds of layers that are linked to each other by a substance called as collagen. if these collagen cross links between the layers are lost due to keratoconus, there is a progressive corneal thinning and stretching which progresses often in both eyes. The cornea bulges forwards into a irregular cone shape causing distortion of image.
The eye develops astigmatism and myopia and vision becomes severely blurred.


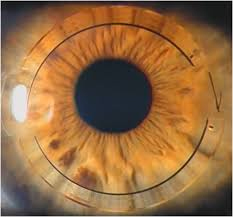 This is a newer surgical treatment for mild to moderate keratoconus. In this surgery, fine
plastic implants are placed in the peripheral cornea, which helps flatten the central cornea,
thereby improving the unaided vision. Patients are able to return back to normal glass wear
or comfortable contact lens wear post treatment. This procedure is painless and simple to
perform. The surgery is performed under topical anesthesia using the
fem to second laser, and takes only 5 -10 minutes per eye.
This is a newer surgical treatment for mild to moderate keratoconus. In this surgery, fine
plastic implants are placed in the peripheral cornea, which helps flatten the central cornea,
thereby improving the unaided vision. Patients are able to return back to normal glass wear
or comfortable contact lens wear post treatment. This procedure is painless and simple to
perform. The surgery is performed under topical anesthesia using the
fem to second laser, and takes only 5 -10 minutes per eye.  With advancement in corneal surgical techniques, it is now possible to selectively
remove the anterior layers from the cornea and replace it with donor tissue to
restore its anatomy and function. Deep anterior lamellar keratoplasty (DALK) is
one such procedure wherein the host corneal endothelium is retained, and anterior
corneal tissue is replaced with normal thickness donor tissue. As the host
endothelium is retained there is no risk of rejection, and steroids have to be
given only for a short duration of time. However DALK surgery requires more
surgical expertise compared to the traditional full thickness keratoplasty, and hence
performed by only well trained corneal surgeons all over the world.
With advancement in corneal surgical techniques, it is now possible to selectively
remove the anterior layers from the cornea and replace it with donor tissue to
restore its anatomy and function. Deep anterior lamellar keratoplasty (DALK) is
one such procedure wherein the host corneal endothelium is retained, and anterior
corneal tissue is replaced with normal thickness donor tissue. As the host
endothelium is retained there is no risk of rejection, and steroids have to be
given only for a short duration of time. However DALK surgery requires more
surgical expertise compared to the traditional full thickness keratoplasty, and hence
performed by only well trained corneal surgeons all over the world.